How Alcoholic Drinks Leads to Liver Disease: An Overview
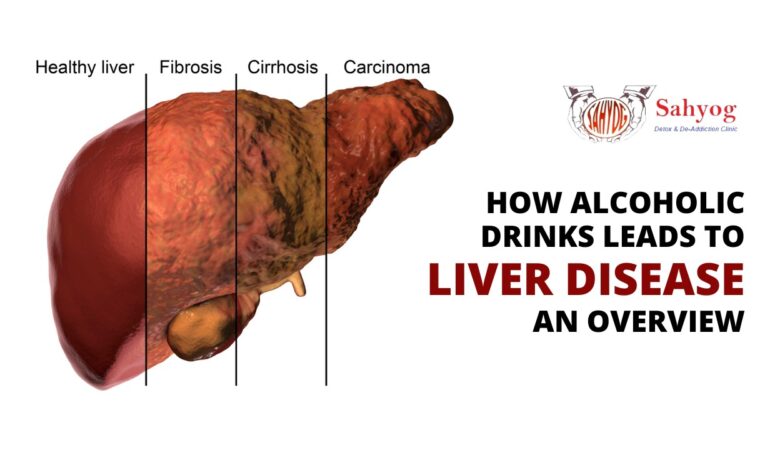
Your liver is one of the most important organs in your body, performing critical functions like breaking down toxins, hormones, and drugs, so they can be flushed out of your system. Unfortunately, it can also be seriously damaged by alcohol consumption and other lifestyle factors, leading to alcoholic liver disease (ALD). In this article, we’ll take a look at what happens in the liver during ALD and some of the symptoms that are caused by this dangerous condition. Alcoholic liver disease can occur in people who consume alcohol heavily, even if they don’t have hepatitis or other liver conditions. As many as one in four heavy drinkers develop fatty liver disease and this can lead to end-stage liver disease in 10-20% of cases, according to the National Health Service (NHS). This article will provide an overview of how alcoholism leads to liver disease and what can be done to protect yourself from it. Alcoholic Liver Disease (ALD) ALD is a term used to describe the damage that chronic alcohol abuse can cause to your liver. The three main types of ALD are fatty liver, alcoholic hepatitis, and cirrhosis. Fatty liver is the earliest stage of ALD and is characterized by an accumulation of fat in the liver. Alcoholic hepatitis is a more serious stage of ALD and is characterized by inflammation of the liver. Cirrhosis is the most serious stage of ALD and is characterized by scarring of the liver. It is difficult to know how long it will take for someone with ALD to develop cirrhosis because many factors determine the progression of the disease, including how much they drink on average per day and how often they binge-drink. Someone who drinks two or more glasses of wine per day may experience signs of alcoholic liver disease within four years, while someone who drinks one glass per day may not experience signs for 20 years. People with other health problems are also at risk for developing ALD sooner than people without any other health problems. For example, those with diabetes have been found to be at risk of developing fatty liver even if they drink moderately. Those with chronic viral hepatitis have also been found to be at risk of developing cirrhosis. Some medications like acetaminophen (Tylenol) can increase the risk of liver injury if taken regularly in large quantities. Furthermore, people who drink more than six alcoholic beverages per week should talk to their doctor about taking extra vitamin B-12, since this vitamin helps protect against some damage done by drinking too. Fibrosis and Cirrhosis Alcoholism is a common cause of liver disease. The first step in the development of alcoholic liver disease is fatty liver, in which excess fat builds up in the liver. If alcohol consumption continues, inflammation and cell death occur, leading to fibrosis. Fibrosis is the build-up of scar tissue that replaces healthy tissue. This scarring can eventually lead to cirrhosis, which is the final stage of alcoholic liver disease. Cirrhosis is characterized by widespread scarring that makes it difficult for the liver to function properly. Damage to the liver may result in jaundice (yellowing of skin), ascites (fluid accumulation), bleeding from varices (enlarged veins), or hepatic encephalopathy (confusion). Cirrhosis can also result in heart failure or kidney failure. Liver transplants are sometimes performed if these complications develop. However, there is no way to stop the progression of alcoholic liver disease once it has started. Treatment usually focuses on slowing down this progression with abstinence from alcohol and monitoring blood sugar levels for those who have diabetes. For many people with severe alcoholism-related liver damage, there is not much that can be done besides waiting until the organ fails completely. In these cases, transplantation is often recommended. Transplantation procedures take a donor liver from someone who died recently and use it to replace the recipient’s diseased liver. Success rates for transplantation vary, but typically range between 40% and 80%. Some patients may only need one transplant, whereas others will need multiple due to recurrence of the condition or because their bodies reject their new livers as foreign objects. Acute Liver Failure Alcohol is a common cause of acute liver failure. In the United States, alcoholic liver disease is the most common cause of acute liver failure. Alcoholism can lead to fatty liver, hepatitis, and cirrhosis. Fatty liver is the earliest stage of alcoholic liver disease and can be reversed with abstinence. If alcoholic liver disease progresses to hepatitis, the damage is more difficult to reverse. Cirrhosis is the most advanced stage of alcoholic liver disease and is irreversible. The only treatment for cirrhosis is transplantation. A person who has developed chronic liver disease will develop other complications such as hypertension, diabetes mellitus, oesophageal varices (oesophageal veins), or hepatic encephalopathy (confusion). In alcoholics without chronic liver disease, mortality may be higher in women than in men because women are at greater risk for breast cancer and other cancers that account for some mortality difference between men and women. Men with alcoholic liver disease have an increased risk of cardiovascular disease and colon cancer. Liver transplants offer an alternative to abstinence from alcohol, but there is a shortage of donor organs. Liver disease can also be caused by viral hepatitis, obesity, exposure to industrial toxins and prolonged use of medications that include acetaminophen. The two main treatments for alcoholic liver disease are abstinence from alcohol or a partial removal of the organ with a transplant if someone is eligible. However, people who have a history of alcoholism are not usually considered eligible candidates for surgery unless they’ve abstained from drinking long enough beforehand to rule out severe heart problems and certain cancers like leukaemia. Hepatomegaly Syndrome Alcoholism is a major cause of liver disease and can lead to a serious condition called hepatomegaly syndrome. This syndrome occurs when the liver can no longer function properly and the kidneys begin to fail. Symptoms of hepatomegaly syndrome include fatigue, nausea, weight loss, and jaundice. If left untreated, this